Novel coronavirus (COVID-19) infections and deaths could increase or decrease substantially in the coming months, depending on how many Iowans practice social distancing or wear personal protective equipment (PPE) routinely in public, according to a modeling app designed by University of Iowa faculty and graduate students.
Six professors of biostatistics or epidemiology collaborated on the model, while a group of graduate students worked on the app and translated materials for a Spanish-language version. The university’s College of Public Health COVID-19 Response Team “developed this tool as a free public service to state and local policymakers, business leaders, and others to assist in guiding the community response to the coronavirus pandemic.”
This incredibly useful resource was derived from publicly-available data, so is not subject to restrictions on release state government imposed as part of the contract the Iowa Department of Public Health and UI College of Public Health signed in April to develop Iowa-specific modeling for COVID-19. Governor Kim Reynolds and state health officials largely ignored that modeling when drafting plans to reopen businesses and venues in May and June, saying “real-time data” was informing such policies.
HOW THE APP WORKS
A video tutorial on the front page of the website explains how to enter assumptions into the app. Users can see how implementing two kinds of “nonpharmaceutical interventions” (social distancing and universal PPE) would affect the number of COVID-19 infections, hospitalizations, or deaths over time. The app can be adjusted to account for the timing of the interventions, how effective PPE is at limiting transmission of the virus, and the share of Iowa’s population that follows social distancing or PPE recommendations.
All graphs start with a “current trajectory” trending downward, reflecting the most recently available data. The researchers note that during this first year of the pandemic, “we do not have direct evidence either for or against seasonal patterns of COVID-19 infections,” which would mirror the long-observed seasonality of other coronaviruses. Consequently, it’s not clear whether Iowans’ behavioral changes or seasonal effects have mostly driven the decline in transmission.
Users can select one of several variables and adjust the dates or other parameters as desired. The graph will then show how one or more scenarios (appearing as lines in different colors) compare to the current trajectory (always red). I enclose some examples from my early attempts to play around with the tool.
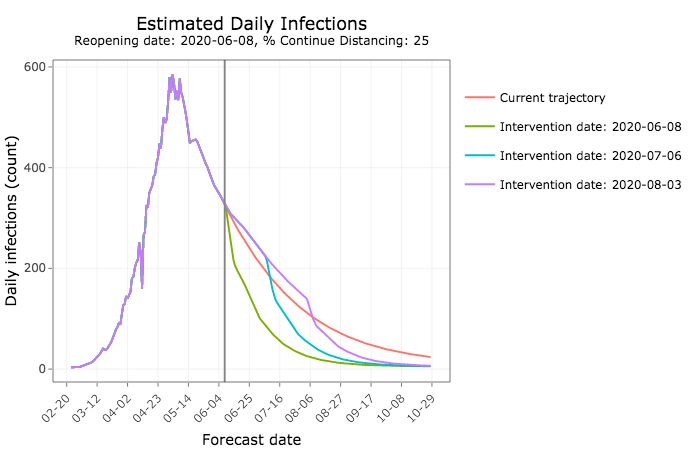
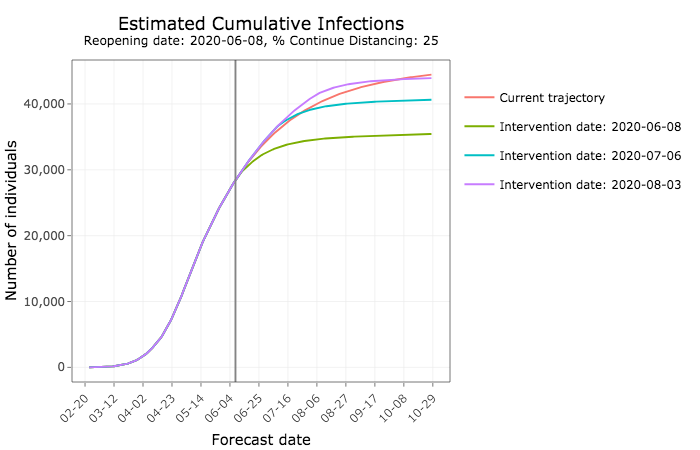
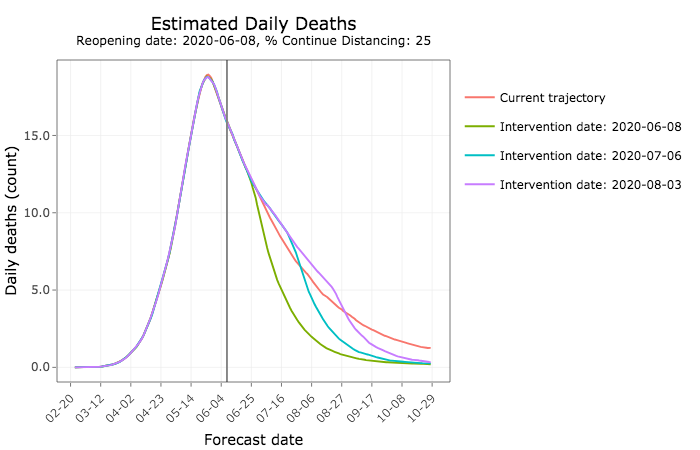
You can see here that the earlier state officials encourage universal use of PPE, the more infections would drop below the number predicted with no new interventions, assuming social distancing is relaxed today (June 8).
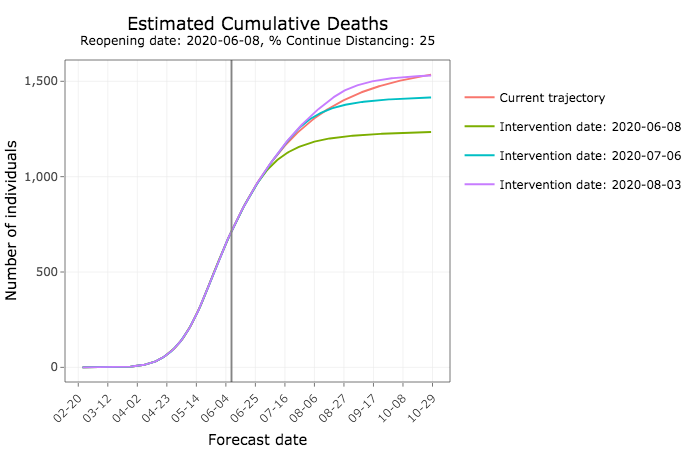
By October, Iowa could see thousands fewer cumulative infections under that policy.
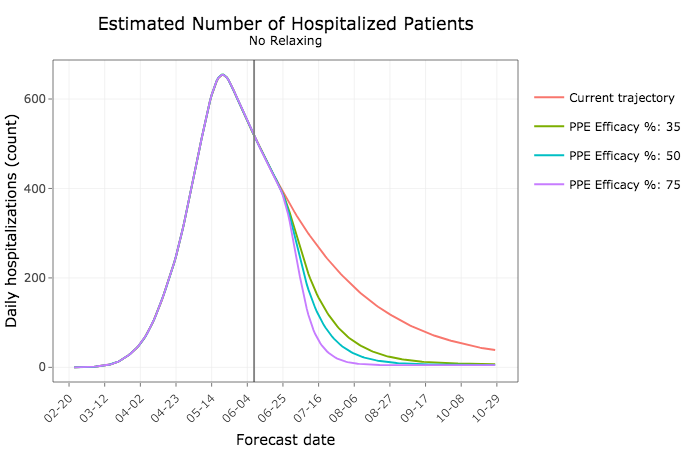
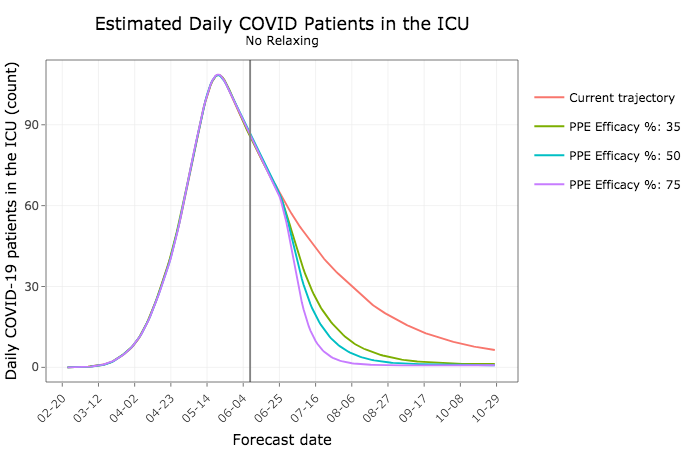
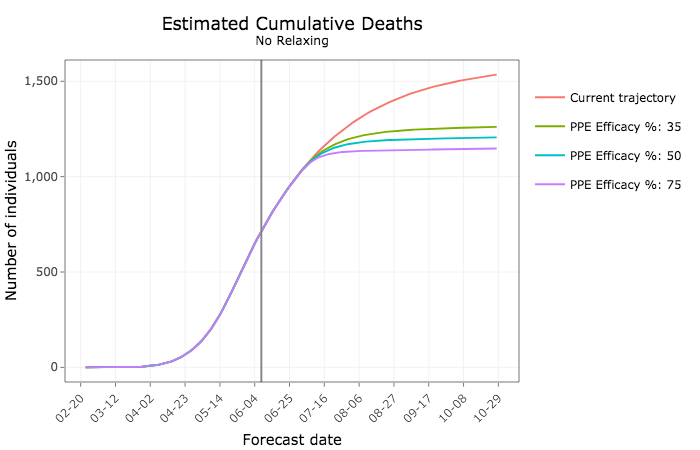
The next two graphs show how more widespread use of PPE would lead to fewer Iowans being hospitalized or in intensive care units. The lines assume different rates of effectiveness–that is, how well the face shields prevent virus transmission.
Hundreds fewer Iowans would die in the coming months under such an approach, the model predicts.
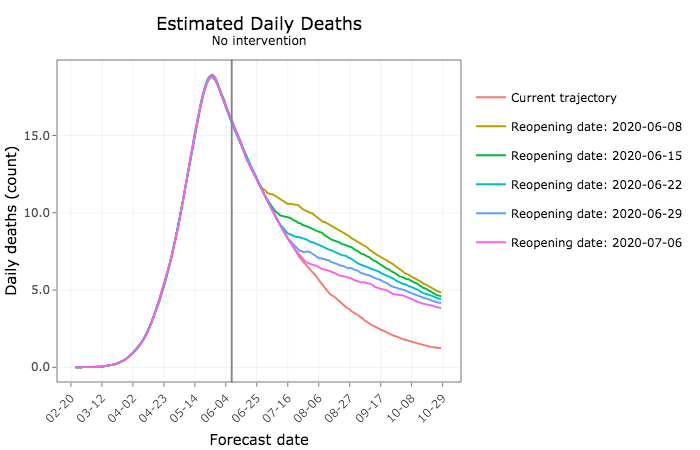
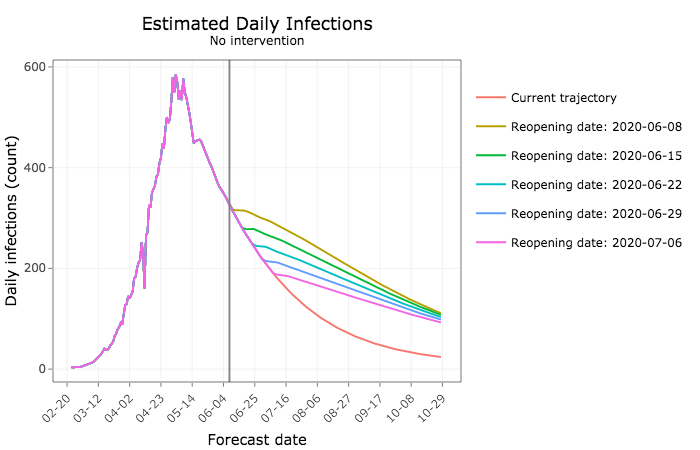
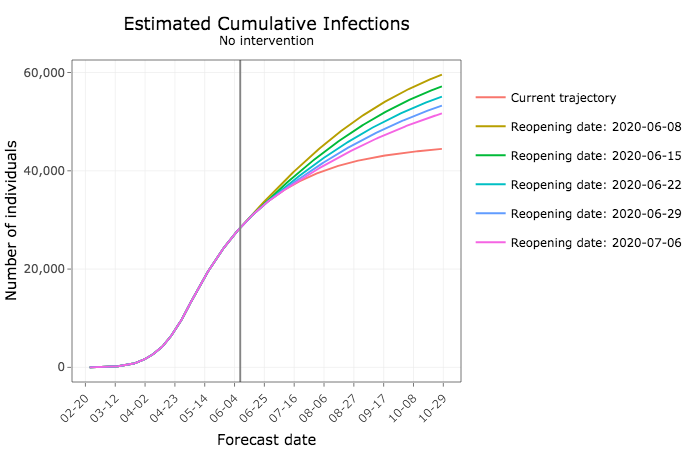
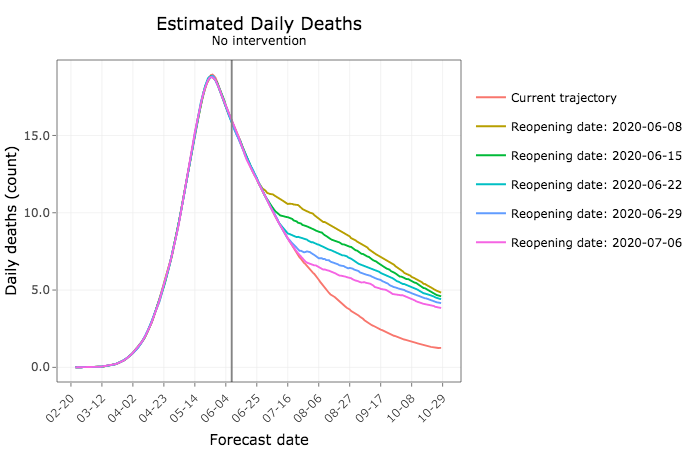
On the flip side, relaxing social distancing without further interventions to reduce transmission would lead to substantially more daily new COVID-19 infections. The sooner Iowans go back to their pre-pandemic habits, the more cases are expected.
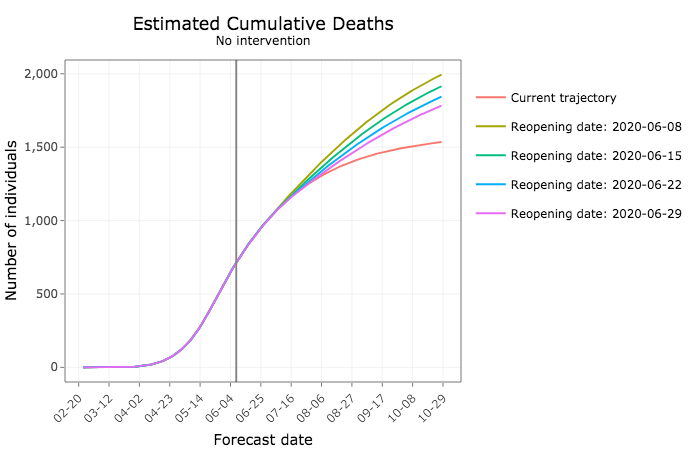
In the coming months, tens of thousands more Iowans would become infected.
And more Iowans would die from COVID-19.
But PPE would reduce the expected number of deaths, even if social distancing is relaxed today. The sooner Iowa moves in that direction, the more lives could be saved.
STATE OFFICIALS IGNORED PREVIOUS CALLS TO PROMOTE FACE SHIELDS
In their final report submitted to the Iowa Department of Public Health on May 26 (enclosed in full below), the university researchers advised that “the widespread use of face shields provides a recourse for safely relaxing social distancing measures.” They also warned,
The relaxation of interventions to contain COVID-19 too early is expected to lead to a large increase in daily infections. Absent any additional measures to keep the outbreak from spreading, such an approach is still expected to yield more infections and hence deaths than more intensive interventions.
The governor and top public health officials have declined to recommend universal use of face coverings. Instead, the governor has said Iowans in vulnerable groups may want to take that precaution, while others may bring a mask with them in case they find themselves in a situation where social distancing is not possible, such as at an outdoor concert.
The Iowa Department of Public Health has published guidance on sewing cloth masks as well as guidance on “wearing cloth face coverings in public places where social distancing measures are difficult,” but has not promoted face shields.
Many health experts including some University of Iowa medical school faculty consider face shields more effective PPE for several reasons.
While medical masks have limited durability and little potential for reprocessing, face shields can be reused indefinitely and are easily cleaned with soap and water, or common household disinfectants. They are comfortable to wear, protect the portals of viral entry, and reduce the potential for autoinoculation by preventing the wearer from touching their face. People wearing medical masks often have to remove them to communicate with others around them; this is not necessary with face shields. The use of a face shield is also a reminder to maintain social distancing, but allows visibility of facial expressions and lip movements for speech perception.
Most important, face shields appear to significantly reduce the amount of inhalation exposure to influenza virus, another droplet-spread respiratory virus.
Susan Nelson published a tutorial here last month, with photos, showing how to make your own face shield.
ANOTHER RESOURCE PROJECTS IOWA’S TRANSMISSION RATE, DEATHS
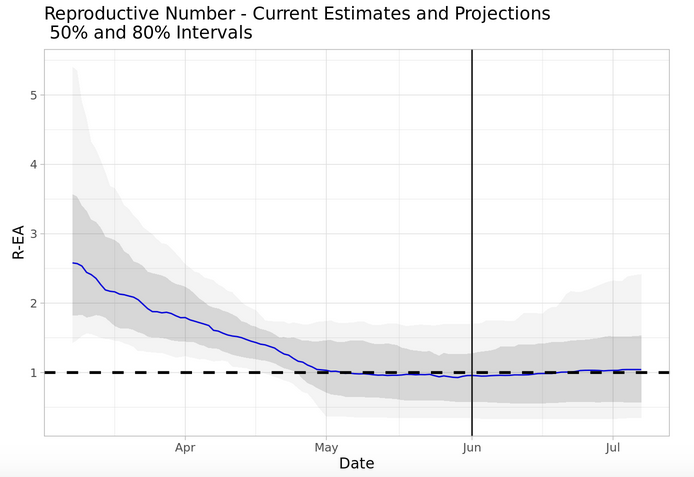
The “other work” page of the new modeling app’s website links to Assistant Biostatistics Professor Grant Brown’s own modeling to project COVID-19 deaths and the “reproductive number” for Iowa. That site explains,
Interventions to control infectious diseases strive to drive the “reproductive number” below 1. While this quantity comes in many forms, and is derived in many ways for different models, in general it captures the number of secondary infections expected per infectious individual. When this number falls below 1, the spread of the disease is expected to slow and stop, while values greater than 1 indicate that the disease is likely to continue to spread exponentially until some other phenomenon interrupts transmission (additional interventions, natural behavioral changes, a lack of susceptible individuals).
Brown’s latest automatically generated report, dated June 7, indicates that Iowa’s “reproductive number” could be either above or below 1, the threshold for uncontrolled spread. There is a 50 percent chance the number falls within the dark shaded area and an 80 percent chance it falls within the range shown in light gray.
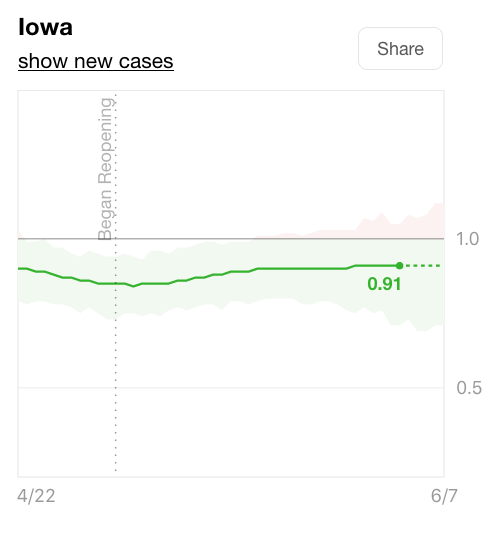
Using different modeling techniques, the Rt live website currently projects that Iowa’s reproductive number is below 1, though the confidence interval includes values above 1.
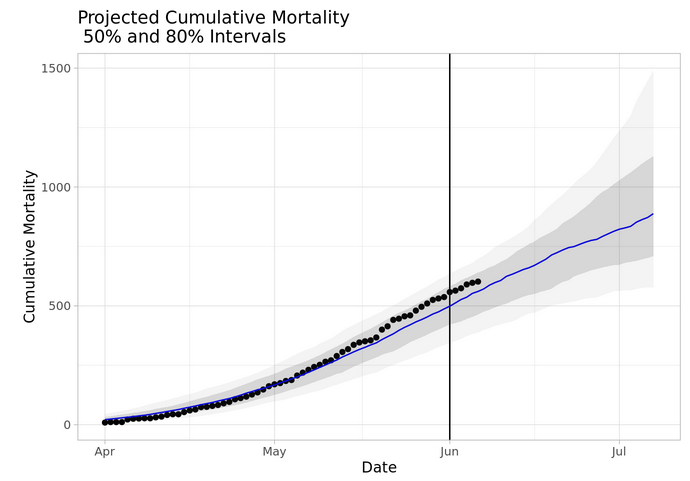
Brown’s latest projection suggests total COVID-19 deaths could reach 800 by the end of this month, with a 50 percent chance the death toll will fall in a range between roughly 700 and 1,100. At this writing, the state reports 612 Iowans have died of the virus.
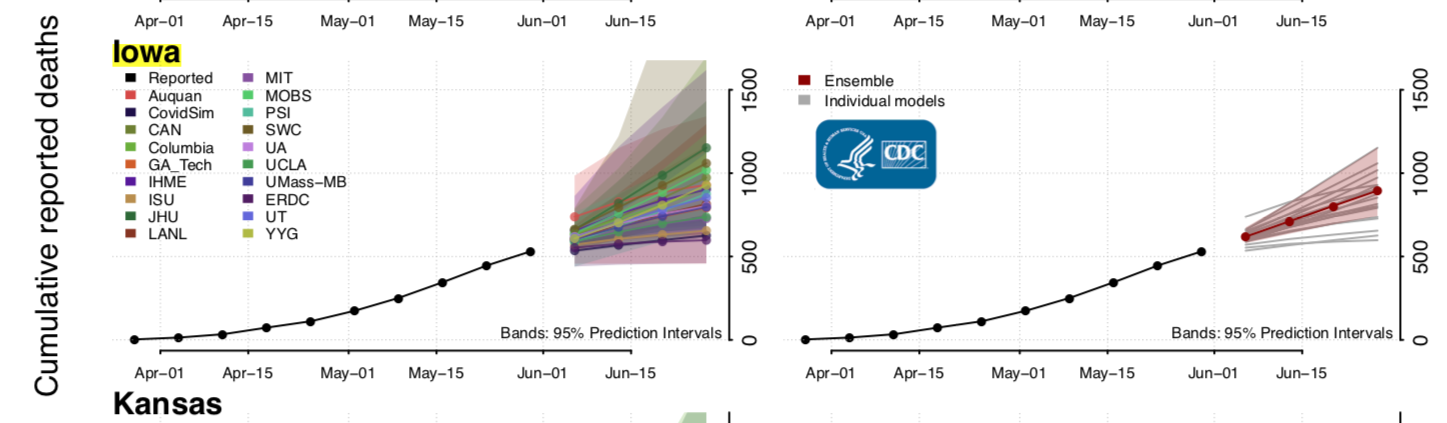
The governor and top public health officials have characterized models as inferior to “real-time data” because models are “based on assumptions at a certain point in time” and are merely “an estimate of what we might see.” For what it’s worth, about 20 other models compiled by the U.S. Centers for Disease Control concur that hundreds more COVID-19 deaths are likely in Iowa during the coming month.
MODEL SUGGESTS “VERY LARGE SECOND PEAK” POSSIBLE THIS FALL
The new website devotes a page to discussing seasonal effects in COVID-19 spread. Researchers caution that this factor is unknown at present.
However, what we are finding in our modeling results is that if COVID-19 does indeed match the seasonality of other HCoVs, then without strong mitigation measures, we should expect a very large second peak starting somewhere around October to December that will dwarf the epidemic curve that we have seen in 2020.
If COVID-19 does end up displaying strong seasonal effects, then the decreasing transmission probability we have seen is not due to behavioral changes, or at least not entirely due to this, but rather is due to the seasonal decline in transmissibility. This implies that we will need to take more drastic measures in the late fall to maintain COVID-19 cases at a manageable level without overburdening the healthcare system. According to our preliminary results, it is unlikely that our society will be able to quarantine at a rate necessary to suppress the second wave to manageable levels, but rather will need to supplement quarantining with universal PPE. However, our preliminary results do show that if PPE is applied with a high compliance rate, the second peak can be effectively minimized to a low, safe level.
We expect that the next few months will shed light on whether COVID-19 is highly seasonal.
The worst flu pandemic in U.S. history was more deadly during its second wave in the fall of 1918. But health professionals of that era didn’t have the resources or treatment options available today. Why do the UI researchers project a wave this fall might strain the health care system? The website notes,
In contrast to early 2020, by the time the second peak begins in late 2020, COVID-19 will have dispersed thoroughly throughout the population while only having infected less than 5% of the population. It will thus be in a prime position to have a maximal impact as the high HCoV [human coronavirus] season begins, thereby leading to a second peak which will be more severe than the first.
I encourage all Iowans to spend some time with the app. Then get hold of (or make your own) face shield to wear during public outings.
___________
Appendix: Final report University of Iowa researchers submitted to the Iowa Department of Public Health on May 26