Less than 24 hours after declaring “the state remains open for business” and asserting that Iowans could address the spread of novel coronavirus (COVID-19) “without me ordering these businesses to close,” Governor Kim Reynolds issued a “State of Public Health Disaster Emergency.” Her March 17 proclamation requires Iowa restaurants to provide “drive-through, carry-out, and delivery only” and temporarily closes fitness centers, theaters, casinos, senior citizen centers, while banning all gatherings of more than ten people.
Political leaders around the country have accelerated steps to force “social distancing” as the threat posed by COVID-19 comes into focus. The Iowa legislature adjourned for at least 30 days after passing resolutions directing funds toward health care needs and giving Reynolds “broad authority to run state government.”
New analysis by health researchers shows why scientists have been calling for more aggressive policies to limit social interaction. Our medical infrastructure cannot accommodate the expected surge in patients needing hospitalization for severe COVID-19 infections.
A March 16 report by more than 30 scientists at Imperial College in London modeled several approaches to containing COVID-19. The researchers concluded that various interventions could vastly reduce fatalities and keep hospitals from being overwhelmed, but those forms of social distancing “will need to be maintained until a vaccine becomes available (potentially 18 months or more) – given that we predict that transmission will quickly rebound if interventions are relaxed.”
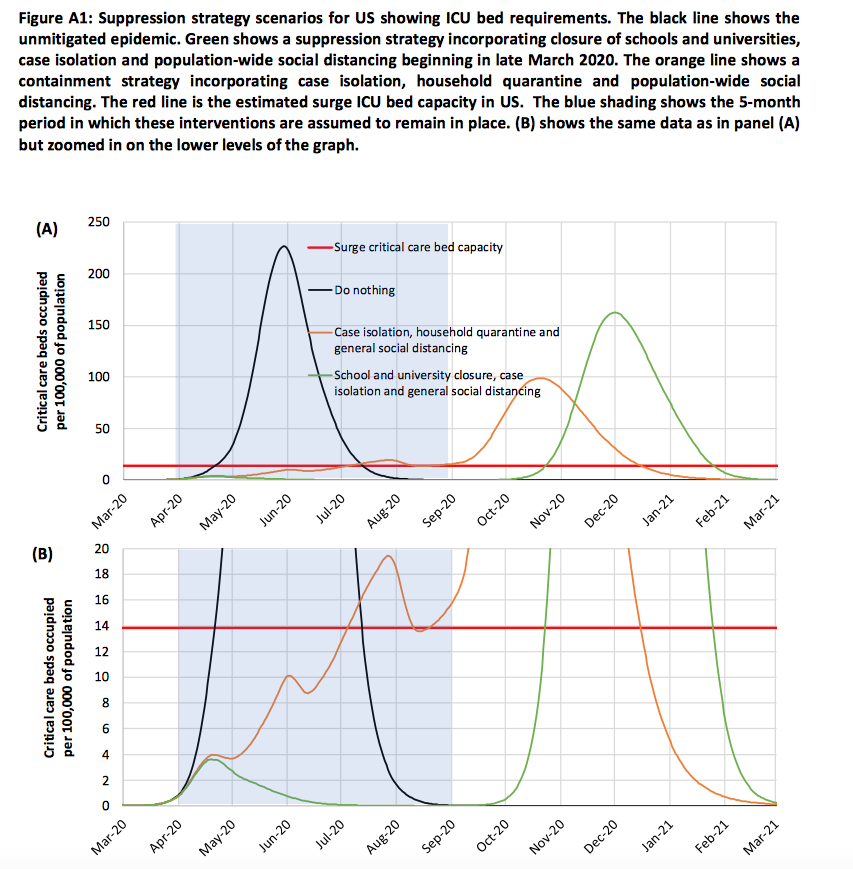
Here’s one table from that report. The red line represents intensive care unit (ICU) capacity in the United States. Even with some interventions, patients needing treatment are projected to exceed the number of available beds by the late summer.
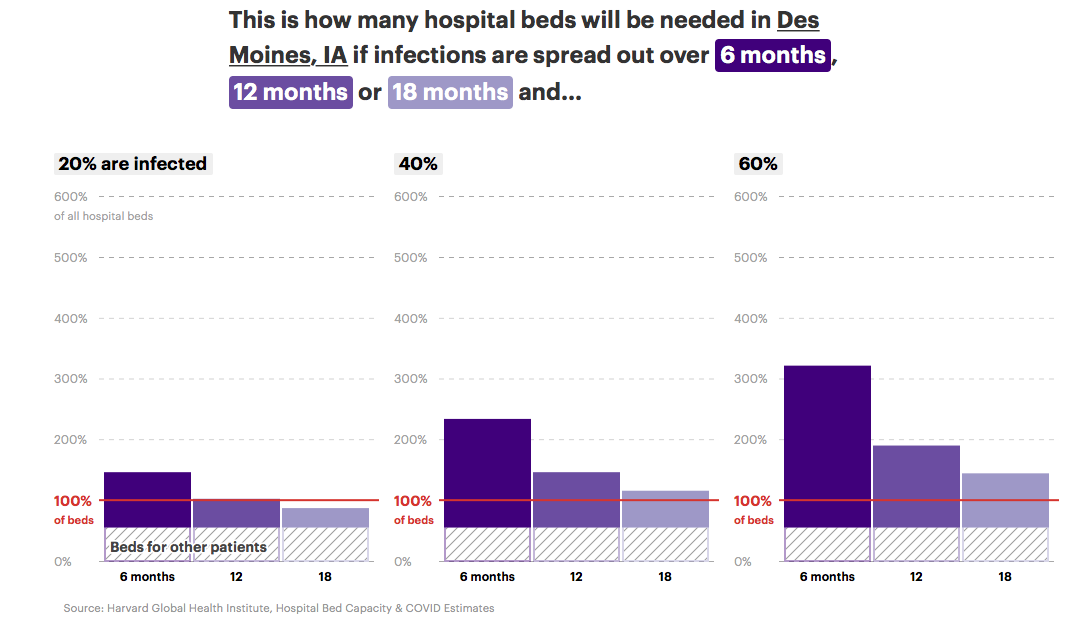
Bringing it closer to home, ProPublica’s Annie Waldman, Al Shaw, Ash Ngu, and Sean Campbell published a terrifying set of maps and tables based on “new data released by the Harvard Global Health Institute.” To illustrate stress on hospital resources across the country, they project nine scenarios, reflecting how many people acquire COVID-19 infections (20 percent, 40 percent, or 60 percent of the U.S. population) and how quickly the virus reaches that share of the population (over six months, twelve months, or eighteen months).
Spreading out the infections over a longer period is essential, these graphics show.
I plugged in Iowa’s largest metro areas to get a sense of how bad things could get here. The Des Moines area had 2,760 total hospital beds in 2018, of which 170 were in intensive care units. About 15 percent of some 1.1 million people in the region served by Des Moines area hospitals are over age 65.
In the moderate scenario, in which 40% of the adult population contracts the disease over 12 months, Des Moines, IA would be among the regions that would need to expand capacity.
It is estimated that about 8% of the adult population would require hospital care. In a moderate scenario where 40% of the population is infected over a 12-month period, hospitals in Des Moines, IA would receive an estimated 72,500 coronavirus patients. The influx of patients would require 2,420 beds over 12 months, which is 2 times times the number of available beds in that time period. The Harvard researchers’ scenarios assume that each coronavirus patient will require 12 days of hospital care on average, based on data from China.
In the Des Moines, IA region, intensive care units would be especially overwhelmed and require additional capacity. Without coronavirus patients, there are only 76 available beds on average in intensive care units, which is 6.8 times times less than what is needed to care for all severe cases.
In Cedar Rapids, only 44 of 800 total hospital beds are in ICUs. Some 16 percent of the area population (about 308,000) are over age 65. “In a moderate scenario where 40% of the population is infected over a 12-month period, hospitals in Cedar Rapids, IA would receive an estimated 19,700 coronavirus patients. The influx of patients would require 660 beds over 12 months, which is 180 percent of times the number of available beds in that time period.” The ICU beds typically available would be 6.5 times “less than what is needed to care for all severe cases.”
Remember, those numbers don’t reflect the worst-case scenario. That’s the middle-of-the-road projection.
Iowa City’s outstanding hospital facilities would be overwhelmed as well, the analysis found. The facilities have 1,410 total hospital beds, including 150 ICU beds. Some 15 percent of about 357,000 residents in the service area are over age 65. Assuming 40 percent of the population acquires COVID-19 over twelve months, Iowa City hospitals “would receive an estimated 23,200 coronavirus patients,” needing 770 beds or 144 percent of the typically available beds. ICU beds would be 2.6 times less than the need.
Here’s how the same moderate scenario would play out in the Quad Cities area:
For Dubuque:
For Waterloo:
For Sioux City:
For Council Bluffs/Omaha:
For Mason City:
The Harvard Global Health Institute researchers focused on hospital beds. Other medical supplies may not be available in sufficient numbers either, some central Iowa hospital officials warned in this March 16 Des Moines Register article by Barbara Rodriguez and Nick Coltrain.
Final note: both mandatory and voluntary social distancing will create considerable economic disruption. For Iowans out of a job because of the downturn, the Des Moines Register’s Donnelle Eller reported on how to apply for unemployment benefits.
Top image: 2012 photo by Corey Coyle of Mercy Medical Center Dubuque, available via Wikimedia Commons.