Joe Gorton is a criminology professor at the University of Northern Iowa. -promoted by Laura Belin
During her March 19 press conference, Governor Kim Reynolds presented her social distancing strategy for protecting Iowa from the novel coronavirus (COVID-19 or SARS-CoV-2) pandemic. Unfortunately, she failed to discuss or even acknowledge any of the significant risks associated with her particular approach.
The purpose of this article is to provide information about the unreported hazards the Reynolds plan incorporates.
DANGEROUS ASSUMPTIONS
In accordance with the Trump administration’s social distancing strategy, Reynolds is asking that people who have Covid-19 symptoms to stay home and follow the recommended treatments for the common flu. Advocates of social distancing assert that self-isolation at home prevents infected persons from transmitting the virus via direct contact with individuals in the wider community. The hypothesized outcome is a reduction in infections that will slow upward trajectory of known illnesses (i.e., flatten the curve).
The governor’s plan relies upon two dangerous and unreported assumptions. The first is that voluntary self-isolation at home people will impede the spread of COVID-19. Second is her implication that infected individuals are not contagious during the asymptomatic (incubation) period of the disease.
Indirect contact
A March 17 article in the New England Journal of Medicine (NEJM) shows that the COVID-19 virus can remain viable on stainless steel and plastic for up to 72 hours, cardboard for 24 hours and copper for 4 hours. The study also revealed that infectious airborne material is viable for up to three hours.
These findings indicate that non-infected individuals can contract COVID-19 indirectly from touching infected material left on a surface by an infected person and then bringing that material into contact with their (or someone else’s) eyes, nose, or mouth. Based on these findings, the Reynolds social distancing plan includes scientifically proven risk of indirectly infecting everyone in an infected person’s household.
Asymptomatic spread
The second hazardous assumption in the governor’s approach is that infected individuals are not contagious during the asymptomatic (incubation) period. This assumption is contradicted by the scientific research. Findings from a University of Texas study (in press) reported, “that time between cases in a chain of transmission is less than a week and that more than 10 percent of patients are infected by somebody who has the virus but does not yet have symptoms.
On March 20, Harvard University’s Coronavirus Resource Center reported, “An analysis from China found that 13% of cases were likely cause by people spreading coronavirus before they started coughing and feeling achy.” In her recent letter published by the New England Journal of Medicine, Dr. Sandra Ciesek, director of the Institute of Medical Virology in Frankfurt, Germany, reports her analysis of 24 airline passengers evacuated from China’s Hubei Province to Frankfurt Germany. According to Dr. Ciesek, “We discovered that shedding of potentially infectious virus may occur in persons who have no fever and no signs or only minor signs of infection.”
A recent pre-printed study (undergoing peer review) conducted by Belgian and Dutch researchers found that 48 percent to 66 percent of infected people from two clusters contracted the infection from someone who was pre-symptomatic. The study’s lead author Caroline Colijn told CNN, “Our analysis would suggest that presymptomatic transmission is pretty commonplace.” Professor Colijn leads the mathematics, genomics and prediction in infection and evolution research group at Simon Fraser University in British Columbia. The study has been posted on MedRxiv, a pre-print server founded by Yale University, the medical journal BMJ and Cold Spring Harbor Laboratory in New York.
A blunt appraisal of the emerging evidence on asymptomatic transmission of Covid-19 was provided by Dr. Michael Osterholm, an epidemiologist and director of the Center of Infectious Disease Research and Policy and the University of Minnesota. Dr. Osterholm told CNN, “We now have conclusive evidence that this disease is also being transmitted through asymptomatic carriers, or people who show no symptoms, and trying to stop that transmission is like trying to stop the wind.”
Centers for Disease Control and Prevention
So far the Centers for Disease Control and Prevention (CDC) seem unimpressed by emerging evidence related to indirect transfer. A March 18 CDC “factsheet” is relatively dismissive of the likelihood indirect transfer stating, “It also may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads.”
The CDC’s current public statement about asymptomatic transmission of the virus is similarly dismissive. “Some spread might be possible before people show symptoms; there have been reports of this occurring with this new coronavirus, but this is not thought to be the main way the virus spreads.”
The disparity between emerging scientific findings and statements from the CDC has not gone unnoticed by researchers on the front lines of the pandemic. In a CNN report, Osterholm called for more straightforwardness by public officials.
“At the very beginning of the outbreak, we had many questions about how transmission of this virus occurred. And unfortunately, we saw a number of people taking very firm stances about it was happening this way or it wasn’t happening this way. And as we have continued to learn how transmission occurs with this outbreak, it is clear that many of those early statements were not correct,” he said. “This is time for straight talk,” he said. “This is time to tell the public what we know and don’t know.”
In the same CNN report, Dr. Colijn stated, “If I were writing that CDC webpage today, I would phrase that a little more towards transmission before symptoms show up,” Dr. Ciesek agreed, “I read it before, and I wondered to myself — why are they so sure of this?”
Spreading the virus within families
The primary and most repeated part of the Reynolds plan is for symptomatic individuals to voluntarily confine themselves to their residence. She fails to acknowledge that in most cases this will mean sharing living space with uninfected members of the household.
It is common knowledge that families are the most effective means for spreading a viral contagion. During this pandemic, anyone who resides with an infected person who is voluntarily isolated will be at high risk of contracting the infection. This is especially true given the likelihood of contagions via indirect contact.
The effect of governor’s social distancing strategy will be to convert our primary social institution into an incubator for COVID-19. In my search of the websites for the governor’s office, the Iowa Department of Public Health, and the Iowa Department of Human Services, I was unable to locate any guidance for households that include a person who has symptoms associated with COVID-19.
MISSING ELEMENTS
There is no doubt that a social distancing strategy is a necessary part of combatting the COVID-19 pandemic. Properly applied, it should eventually reduce the rate of transmissions (flatten the curve) and possibly prevent exponential increases in infections. But necessary is not the same as sufficient. To better protect Iowans, the governor must take two actions. First, she must be more transparent with her metrics for success. Second, she should broaden her strategy to include a greater emphasis on community based interventions.
Complete and accurate information
During the past week, I’ve watched, in their entirety, five of the governor’s press conferences about COVID-19. Unlike President Donald Trump, Reynolds has consistently conveyed a sense of even tempered confidence. Her performance makes it easy to conclude that her administration is doing everything possible to combat the Covid-19 pandemic.
Impression management notwithstanding, there are significant problems with the lack of information and transparency in the governor’s press conferences. Here are a few examples. When reporters ask for the available amounts of personal protective equipment or ICU beds, the governor and her team consistently refuse to give numbers or specific status reports. Instead, they give self-serving descriptions of what they are doing to build supply. Alternatively, they lean on the dissembler’s best dodge by saying the numbers are “constantly changing.”
Questions about statistical modeling used for projections about future infection rates are especially troubling. In one press conference, Iowa Department of Public Health Deputy Director Sarah Reisetter claimed, “We do not have modeling like that that we would show at this time,” to which she added, “we are watching what is happening in other states.”
When asked about the likelihood of asymptomatic spread, Reynolds and others have given the non-response that the infection is most like to be spread by people who are symptomatic. A more honest answer to that important question would have referred to some of the above findings on asymptomatic spread of COVID-19.
One of the most concerning examples of questionable information came from Reynolds’ explanation for the growing number of Covid-19 infections. On March 23, she asserted that a single-day increase from 90 to 105 infections was a product of increased testing. At best, her answer amounts to dissembling. The administration’s stated policy is to limit testing to:
Hospitalized patients with fever and respiratory failure and no alternate diagnosis. Hospitalized older adults (those older than 60) with fever and respiratory symptoms and chronic medical conditions. Any person with household contact with a laboratory-confirmed case of COVID-19 in the 14 days before becoming ill with fever or respiratory symptoms. Any person with a history of international travel to a country with a level 3 CDC travel health warning or who has taken an international cruise in the 14 days prior to becoming ill with fever and respiratory symptoms and no alternate diagnosis.
Reisetter told reporters on March 20 that testing was mainly limited to people who are hospitalized. Given the narrow testing criteria, increases in confirmed infections point to growing prevalence of the virus. There is no good reason for the governor to claim otherwise.
Flattening the curve: honest transparent metrics matter
To her credit, Reynolds is pushing as hard as she can for all Iowans to practice social distancing. She rightfully explains that rigorous social distancing will help slow the spread of the virus. That in turn will mitigate the growing burden the infection is placing upon our health care system. It is not helpful, however, that her discussion of social distancing does not include appropriate metrics for evaluating progress lack of progress in flattening the curve.
According to my readings, flattening the curve refers to the reducing the exponential increase in infections. The quantitative criteria for exponential growth is the number of days it takes for infections to double. According to a March 17 report in Infection Control Today, the COVID-19 doubling time in the United States is about six days.
A recent analysis of social distancing models published by Imperial College London’s COVID-19 Response Team used an estimated doubling time of 2.4 days.
Comments from Reisetter (who has no epidemiological or scientific training) suggest that the Reynolds administration is not using exponential modeling to evaluate progress in flattening the curve. During the March 24 news conference, the Des Moines Register’s Jason Clayworth asked about criteria for evaluating progress in flatting the curve. Reisetter gave the following criteria: percent of infected over age 65, percent of hospitalized cases, infected rate per 100,000 over a fourteen-day period, and number of infections in residential settings.
None of those are exponential metrics. Iowa’s State Medical Director Dr. Caitlin Pedati cited the same criteria during the governor’s March 25 media availability.
Even under the best-case scenario, social distancing is not likely to stop an exponential spread of COVID-19. Though it relies upon an admittedly small sample of available data, my rudimentary calculation of infections from March 13 to March 25 suggest a current Iowa doubling time of five days. To place that in context, a fifteen-day doubling time would lead to approximately 1,100,000 infections in nine months.
According to Dr. Anthony Fauci’s recent Congressional testimony, COVID-19 produces a 1 percent fatality rate. At that fatality rate and a starting number of seventeen infections on March 13, a fifteen-day doubling time would produce 11,114 deaths in our state within nine months. The real-world doubling time will probably be closer to five days.
The Cedar Rapids Gazette published an up-to-date graph showing the exponential growth of Iowa’s Covid-19 infections.
Reynolds and her top advisers on this matter should reveal specifically whether they are using exponential (doubling time) numbers to evaluate their progress in flattening the curve. If they are, then they should explain why they have not included that information in their response to reporters’ questions.
If they are not using exponential numbers, then they should explain their reasoning for that decision. The news media should be relentless in continuing this line of inquiry.
Infrastructure for community-based intervention
Reynolds has stated repeatedly that her social distancing goal is to prevent COVID-19 from “crashing” Iowa’s health care system. But given the virus’ probable rate of spread, the declining availability of hospital beds and the use of weak prediction metrics, the current social distancing program is unlikely to achieve that goal.
According to the social distancing analysis the Imperial College London Covid-19 Response Team published on March 16 (emphasis added),
mitigation is unlikely to be feasible without emergency surge capacity limits of the UK and US healthcare systems being exceeded many times over. In the most effective mitigation strategy examined, which leads to a single, relatively short epidemic (case isolation, household quarantine and social distancing of the elderly), the surge limits for both general ward and ICU beds would be exceeded by at least 8-fold under the more optimistic scenario for critical care requirements we examined. In addition, even if all patients were to be treated, we predict there would still be in the order of 250,000 deaths in GB, and 1.1-1.2 million in the U.S.”
The findings from several sources point to the same conclusion: social distancing alone probably will not prevent the pandemic from overwhelming Iowa’s health care system. What is needed then is a mitigation strategy that couples social distancing with new infrastructures of community-based interventions. Building that capacity is the only way to increase the surge capacity of Iowa’s health care system.
Fortunately, there are existing models. A February 13 article in the prestigious medical journal The Lancet shows how China successfully augmented its social distancing strategy through the use of “fever clinics.” According to Bruce Aylward, senior adviser to the Director General of the World Health Organization, China’s network of fever clinics are an important reason that nation has been able to restart its economy.
In this video clip, Dr Aylward, who spent considerable time in the Wuhan Province of China, comments about that nation’s approach to the COVID-19 pandemic.
Working together, Iowa’s public, private and nonprofit entities should create mobile and fixed temporary locations for evaluating individual symptoms, referral for COVID-19 testing, case tracing, assistance with prescriptions, instructions for home care, crisis intervention counseling, separation/isolation/quarantine and other forms of assistance.
COVID-19 community assessment centers need to quickly become part of Iowa’s mitigation plan. Every urban area in Iowa has unused retail properties that can be converted into assessment and isolation centers. Iowa’s National Guard should be deployed to help build and maintain the infrastructure. In fact, our National Guard should already have a plan in place to convert these and other properties into facilities for testing and treatment. An infrastructure of this type will provide significant relief for our health care system and will improve the ability of Iowa to flatten the curve. In addition, it will help us to be prepared prior to the next flu season.
Partnership with organized labor
During one her recent press conferences, Reynolds was asked what she is doing to address the economic hardships social distancing has imposed upon thousands of Iowa families. Her response focused on her discussions with leaders in the business community and financial sector. Notably absent was any acknowledgement of the important role of Iowa’s union will play.
Iowa’s union members and their leadership are a vital part of the economy. They are important partners with organizations such as United Way and other nonprofit agencies. Their knowledge, expertise, community involvement, and volunteer spirit are unrivaled. It’s well known that our governor has no love for labor unions. But at this moment of crisis it is imperative for her to put her politics aside and reach out to one of Iowa’s best resources.
Voluntary social distancing or mandatory shelter in place?
Readers will note that this piece does not address the controversy of voluntary social distancing versus mandatory shelter-in-place orders. During my research, I was unable to locate any research that pointed to one of these methods as being more effective than the other. I believe there are advantages and disadvantages to both.
For now, I favor a voluntary approach that also includes resources for quarantine of particular individuals. My recommendation is for community-based infrastructure, which would include large number of isolation beds so that infected adults can be separated from their families. As a criminologist, I have concerns about widespread restrictions that are probably unenforceable.
FINAL THOUGHTS
Reynolds’ failure to acknowledge the contagion effects of indirect contact and surface spread of COVID-19 is an unconscionable withholding of vital information. That alone could cause many Iowa households to become social incubators for the virus. In China, 80 percent of infections were contracted within families.
The governor is either unaware of, or is purposefully withholding, information on the proper method for calculating of the effects of her social distancing mitigation plan. When reporters probe this area, Iowa Department of Public Health officials consistently fail to discuss well-established exponential criteria for this assessment.
Reynolds’ exclusive reliance on mitigation through social distance ignores the obvious need to create a statewide infrastructure of community-based interventions. Speed is of the essence. With exponential growth, the virus will increase rapidly. A community-based intervention model like the one discussed here will place a much needed speed bump between the pandemic and Iowa’s under resourced health care system. That would buy us time to further build out our capacity to contain the virus.
By contrast, the current approach to mitigation will cause the surge limits on Iowa’s health care system to be exceeded sooner rather than later. It could also leave Iowa vulnerable to an even worse crisis during our winter months.
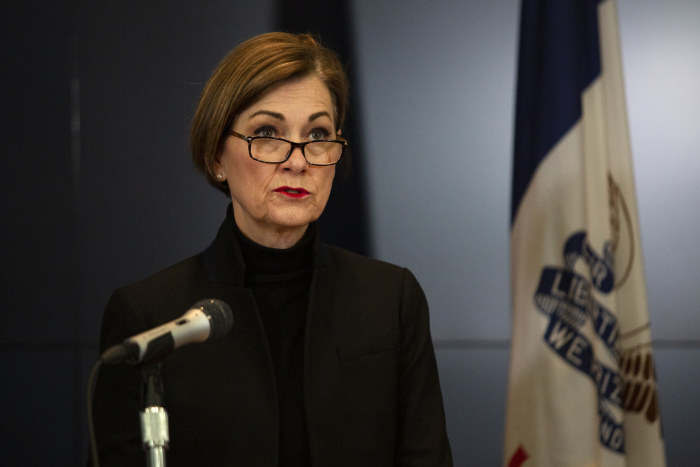
Top photo of Governor Reynolds speaking at her March 25 news conference by Olivia Sun of the Des Moines Register (pool).

1 Comment
Iowa is starting to look impressively clueless...
https://www.sfgate.com/coronavirus/article/states-with-no-shelter-in-place-orders-15166557.php
PrairieFan Tue 31 Mar 2:02 AM