John Morrissey is a native Iowan and longtime Des Moines resident. -promoted by desmoinesdem
Despite promises of huge annual cost savings resulting from Medicaid privatization, Iowa’s medical assistance programs spent more in eleven months of the current fiscal year than during all of the previous fiscal year.
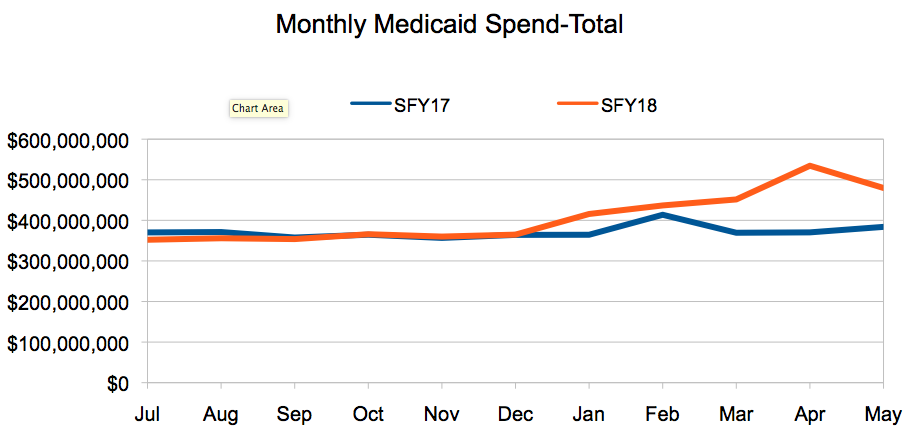
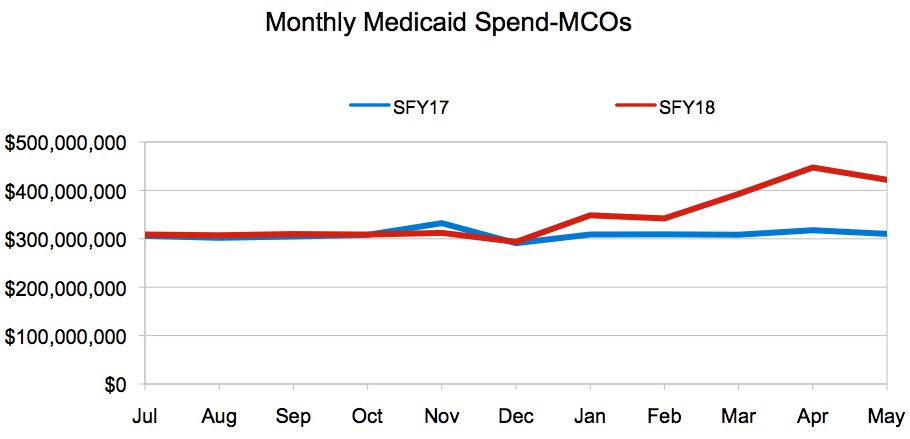
The portion of Medicaid funds paid to managed care organizations (MCOs) at the end of this May increased by $394 million compared to May 2017. The “Fiscal YTD Expenditures by Category of Service” report, published on the Iowa Department of Human Services (DHS) website each month, tracks 74 spending categories. MCO spending, which is running a little more than 9 percent higher so far this year, is tracked on its own line. The remaining 73 expense categories net out to a spending decrease of $10 million compared to May of last year. I put the data into a spread sheet and created these line graphs:
The cost surge at the troubled Medicaid program is mostly on the federal ledger, however, because of the federal-state financing splits that apply to various Medicaid enrollment categories that MCOs serve in Iowa. Total Medicaid spending through eleven months of the current state fiscal year was $4.470 billion. Generally, the state pays 40 percent of the cost, while the federal government pays 60 percent.
The DHS reports indicate much of the increased spending this fiscal year is attributed to the Iowa Health and Wellness Plan, which provides health insurance to low-income adults under our state’s version of Medicaid expansion. The federal government picks up 90 percent of the costs for that enrollment segment.
The outlook for the Medicaid program was much rosier at the end of December, when total spending for the current fiscal year was running nearly $30 million less than at the same period in fiscal year 2017. Medicaid expenses hit the accelerator in January, apparently due to implementation of contract amendments governing how much the MCOs are paid. Expenses have increased steadily since.
Iowa Department of Human Services Director Jerry Foxhoven said the comparison of this year to last is affected by “reprocessing of [capitation] rate changes for previous reporting periods” being made to the MCOs, as well as medical cost inflation. He did not specify how much each factor contributed to the extra spending.
“[The] report includes both standard capitation payments as well as capitation payments that have been reprocessed for a previous reporting period, so the number is inflated,” he wrote in an email.
“That said, there was an increase reflected in the SFY18 capitation payments when compared to the SFY17 capitation payments due to emerging trends associated with rising health care costs impacting the Iowa Medicaid system and would have been absorbed whether there was managed care or not.”
Whatever the cause, the MCOs operating in Iowa have received the additional payments. Contract amendments filed on the DHS website earlier this year indicate that Amerigroup and UnitedHealthcare have agreements with the state to reprocess capitation rates. UnitedHealthcare submitted a revised capitation schedule with its contract amendment. Amerigroup agreed to a risk corridor strategy that apportions additional costs between itself and the state.
It is not clear how the capitation rate reprocessing will affect the cost savings that former Governor Terry Branstad claimed justified the move to private insurers. Iowa Medicaid Director Michael Randol told state officials June 12 that the program has saved $141 million during the current fiscal year. That was apparently based on a comparison of total managed care cost so far this fiscal year with the projected cost trend for the previous state-operated system, which was supplanted in mid-2016. [Editor’s note: Randol did not explain the methodology underlying the savings estimate.]
Foxhoven did not directly answer whether the increased spending has or will have an impact on the state budget.
“Each state with managed care is federally required to develop and certify actuarially sound rates for reimbursement to MCOs. The department works closely with the Department of Human Services Council as well as the legislature to project budgets for each year as well as to inform these entities of projection changes. It is important to note that increased projections are for the Medicaid program as a whole and would be realized in a managed care environment or [fee for service] FFS.”
Under privatization, the state makes set payments, called capitations, to the managed care orgaizations each month for each person enrolled in Medicaid. The MCOs are responsible for using the capitation payments to cover all costs involved in providing medical care to eligible Medicaid enrollees, as well as their administrative costs. If there is money left over, the MCOs get to keep it as hoped-for profits.
The MCOs file dozens of capitation rates with the state, covering the payment the MCO will receive for specific populations and medical conditions. Capitation is supposed to help control medical costs by transferring to the insurance companies some of the financial risk of paying for services.
The health insurance companies who contracted with the state under privatization have been complaining the rates they agreed to were not sufficient to pay the claims they received since the program began. Incomplete financial accounting published by the Iowa Medicaid Enterprise on its website shows the three MCOs that were active during the 2017 fiscal year received $3.6 billion in capitation payments from the state, but suffered uncompensated losses of $457 million when paying for Medicaid services.
The bad news about Iowa’s Medicaid program costs comes even as total enrollment has been rising during the current fiscal year, according to monthly enrollment reports published on the DHS website. About 5,100 more children are covered by the HAWK-I program, and nearly 18,000 more by the Iowa Health and Wellness Plan, compared to July 2017. Traditional Medicaid enrollment has held steady.
Capitation payment rates to the MCOs have been a sticking point between state officials and the insurance companies. Last fall, the companies claimed they were losing hundreds of millions of dollars because the rates were based on flawed actuarial assumptions. One MCO exited the Iowa marketplace because of sustained losses. The DHS subsequently fired its actuarial advisor and announced June 8 that it intends to hire Optumas, an actuarial consulting firm based in Scottsdale, Arizona.
Optumas provided actuarial consultation to Kansas state officials in 2012 when that state filed a waiver with the Centers for Medicare and Medicaid Services to privatize the Kansas Medicaid program. That initial waiver filing was rejected by federal officials because it forgot to include Indian Health Service enrollees and facilities. CMS approved the KanCare waiver four months later, and the Optumas contract with the state of Kansas called for payment of up to $1.7 million for services rendered prior to the rollout of KanCare in 2013.
I sought comment about the Iowa Medicaid spending situation from DHS officials, the governor’s office and the ranking members of the appropriations subcommittee that oversee DHS.
“Negotiations are still ongoing for the new capitation rates for next year and we really don’t have a good idea where they will land,” Democratic State Representative Lisa Heddens, ranking member of the joint Health and Human Services Appropriations Subcommittee, responded by email. “My best guess is between $60 and $100 million state dollars, but that is just a guess. Last year it was a $60 million state increase.”
As to how much of the $100 million savings the privatization effort actually occurred during the first year, or whether the “reprocessing” effort might affect those savings claims, Heddens wrote, “I do not know exactly where the savings are coming from.”
Requests for comment to Medicaid Director Randol and Governor Reynolds’ spokeswoman Brenna Smith, were not returned. The Republican co-chairs of the Appropriations subcommittee, Senator Mark Costello and Representative Dave Heaton, also did not respond. Senator Mark Segebart, co-vice chair of the subcommittee, sent an automated email message saying due to the press of business, he could not respond immediately. Representative Rob Taylor, the other co-vice chair, did not respond. Nor did Senator Amanda Ragan, the ranking Democrat on that committee.